Embedding and supporting your personalised care workforce to tackle health inequalities
It is well known that the availability of good medical and social care is inversely related to need, with people living in areas of deprivation more likely to experience unmet need, poorly coordinated care and a greater reliance on unscheduled services. From a workforce perspective, working in “Deep End” areas is associated with higher levels of stress and burnout and increased staff turnover and problems with recruitment and retention.
This means practical and emotional support for the ARRS PC workforce becomes more important in areas where the highest health inequalities exist. Addressing health inequalities requires strong workforce support.
We have heard numerous challenges around embedding the personalised care workforce.
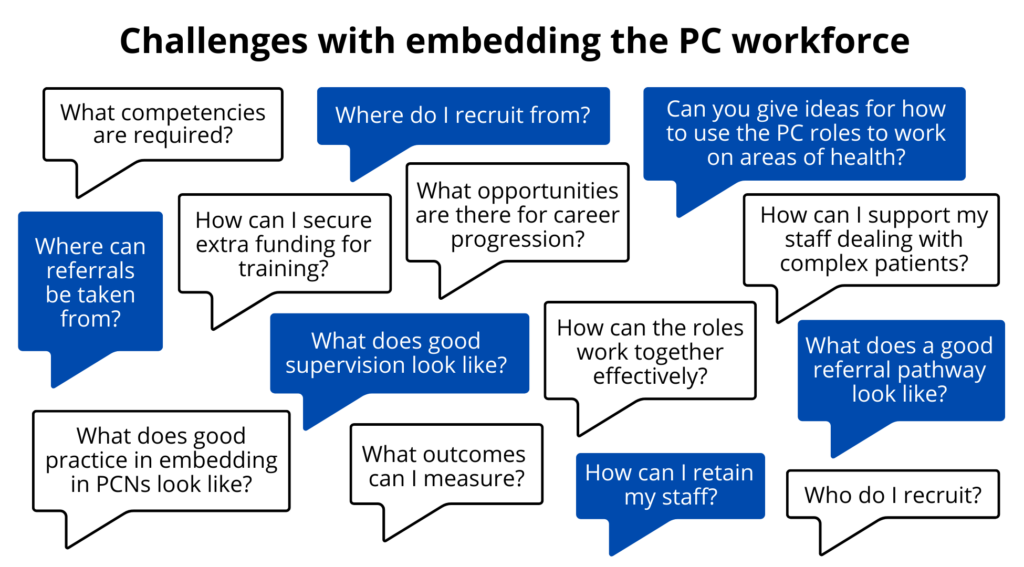
- Be familiar with national and local guidance and resources including local and ICS level Training Hub offers for the personalised care workforce
- Recruitment: think about multiple sources and what local needs and assets are e.g. NHS Careers, local community, PCN or practice staff looking for opportunities
- Diversity and representation: does your workforce represent the community it serves? How can you encourage people from the local community to apply for these roles?
- Retention: what is important to your workforce that will help them stay? How can you find out?
- Career progression: provide opportunities for training and development that align with the workforce’s needs and local priorities e.g. sub-specialisation to meet a specific need
- Supervision: ensure there is allocated protected time for regular supervision and a named contact/duty supervisor should urgent issues arise (more information on this below)
- Funding: what sources of funding are available to support your workforce e.g. local authority, public health, CCG, community chest scheme, innovation schemes
- Do you have clear referral pathways? Are these communicated to those who are referring into the service?
- How are you documenting activity, outcomes and impact?
- Diverse governance and leadership – how inclusive and representative is your PCN?
- Clear values and shared purpose in a coherent system – how do these show up in your PCN’s strategy, communication and overall work?
- Supporting professional development and supervision of ARRS roles and considering team leader / complex case manager
- Understanding of the 3 PC roles with clear and consistent referral criteria- is this easily accessible? How is this communicated to staff?
- Understanding of DES and using it to align with local needs and priorities including health disparities
- 3 personalised care roles are linked in with community assets and multi-sectoral partners. Is there protected time for community engagement and development?
- 3 personalised care roles are embedded effectively alongside other members of the primary care and wider team. Are they part of clinical meetings, MDTs and social events?
- Adequate resources and support including clear induction and job role, protected time for supervision, remuneration proportionate to workload and complexity that is higher in deprived areas
- Opportunities for further training and advocacy to develop specialism and service lead roles
- Health inequalities lead and/or personalised care champions available to provide strategic direction and support
- Forward thinking and developing a one team approach, particularly with the 3 roles.
Some examples:
- Case manager/ ARRS manager
- Social Prescribing manager
- PCN manager
- PCN/local personalised care lead/ Health inequalities lead
- Specialist roles e.g. mental health, children and young people, welfare and legal support
- Data analysis and service delivery
- Community development roles
How can you support career progression opportunities, training, and pathways for your ARRS roles?
Case Scenario
Career progression from SPLW to PCN manager and personalised care lead
Watch back our webinar which includes a case study from Barnsley with a PCN manager and personalised care lead who transitioned from a social prescribing link worker into a leadership and management role and developed a strong personalised care team with an emphasis on regular PCN meetings with all 3 roles, collaborative working, shared learning and reflection and communication and education of all staff.
- Wellbeing scores e.g. ONS4
- Healthcare access and usage e.g. Did Not Attend rate, frequent users, unscheduled care use, hospital admission
- Healthcare experience e.g. mental health and maternity services
Care plans, annual reviews, QOF targets - Physiological indicators e.g. weight, blood pressure, diabetes control, asthma/COPD flare ups
- Uptake of specific interventions e.g. cancer screening, immunisation
- Socio-economic indicators e.g. employment, access to welfare support, foodbanks, secure housing
- Patient satisfaction/feedback
- Case notes review/discussion
- Economic evaluation.
See here a checklist for evaluation (from page 57 onwards)
A note on measuring impact
Many social prescribing and personalised care interventions are complex, requiring innovative, integrated, and multiple methods to measure impact. Current evaluation programmes and studies have several limitations in the methodology used to evaluate these complex interventions. Additionally, most research focuses on short term outcomes, cost-effectiveness, or intermediate interventions rather than looking at long-term benefits or context such as social drivers, capital and responsibility with health, or processes involved such as patient experience and journey.
Additional time to build trust and address complex needs:
- Sufficient numbers and skillset to address needs comprehensively across the local population and minimise staff burnout
- Access to IT systems to document needs, concerns and actions- templates can be helpful to structure entries
- Access to interpreters and resources in multiple languages/modalities
- Regular MDTs with multi-professionals to discuss care holistically and share concerns
- Protected admin time due to higher referrals and documentation that complex consultations can generate
- Processes and protocols and named point of contact to deal with:
– Medical emergencies/urgent queries
– Mental health crises
– Safeguarding, DVA, trafficking
– Emergency accommodation, carer respite - Working relationships with the wider team- primary care, social care, community groups
- Regular supervision and access to debriefs and on the day support
- Opportunities for further training or develop special interests
- Opportunities to work closely with community groups can reduce isolation as well as build important community links and intelligence
- Peer support sessions within the PCN and with neighbouring PCNs to build a local community of practice and share resources and learning.
Case Scenario
Frailty service for patient-centred complex care
A frailty hub takes place every 2 weeks for a practice run jointly by a GP, frailty nurse and a frailty HSCA who has a hybrid role combining social prescribing and care coordination. Before the hub is an MDT with a medicine optimisation pharmacist who carries out a tailored medication review for all patients being reviewed in the hub and suggests recommendations for safe prescribing. Once a month a geriatrician is present to provide input on complex issues.
During the hub, the patient has a one-hour review appointment during which a comprehensive social, nursing and medical care plan is jointly completed. The hub is co-located next to therapy, rehabilitation and social and community services which improves communication and efficiency of multi-agency involvement. The HSCA is well linked into the local community and is able to refer to a range of services such as appropriate patient and carer support groups, social activities, reading on prescription, as well as liaise with social services and carry out welfare checks. If the patient needs blood tests and other bedside tests, then these can be carried out during the appointment.
The service has received very good feedback from patients and staff. For patients it avoids the need to travel between different locations and they can access a wide of range of services conveniently in one place and have more time with professionals. For GPs, it provides continuity of care with longer appointments for the most complex patients and they feel well supported by a team of professionals around them.
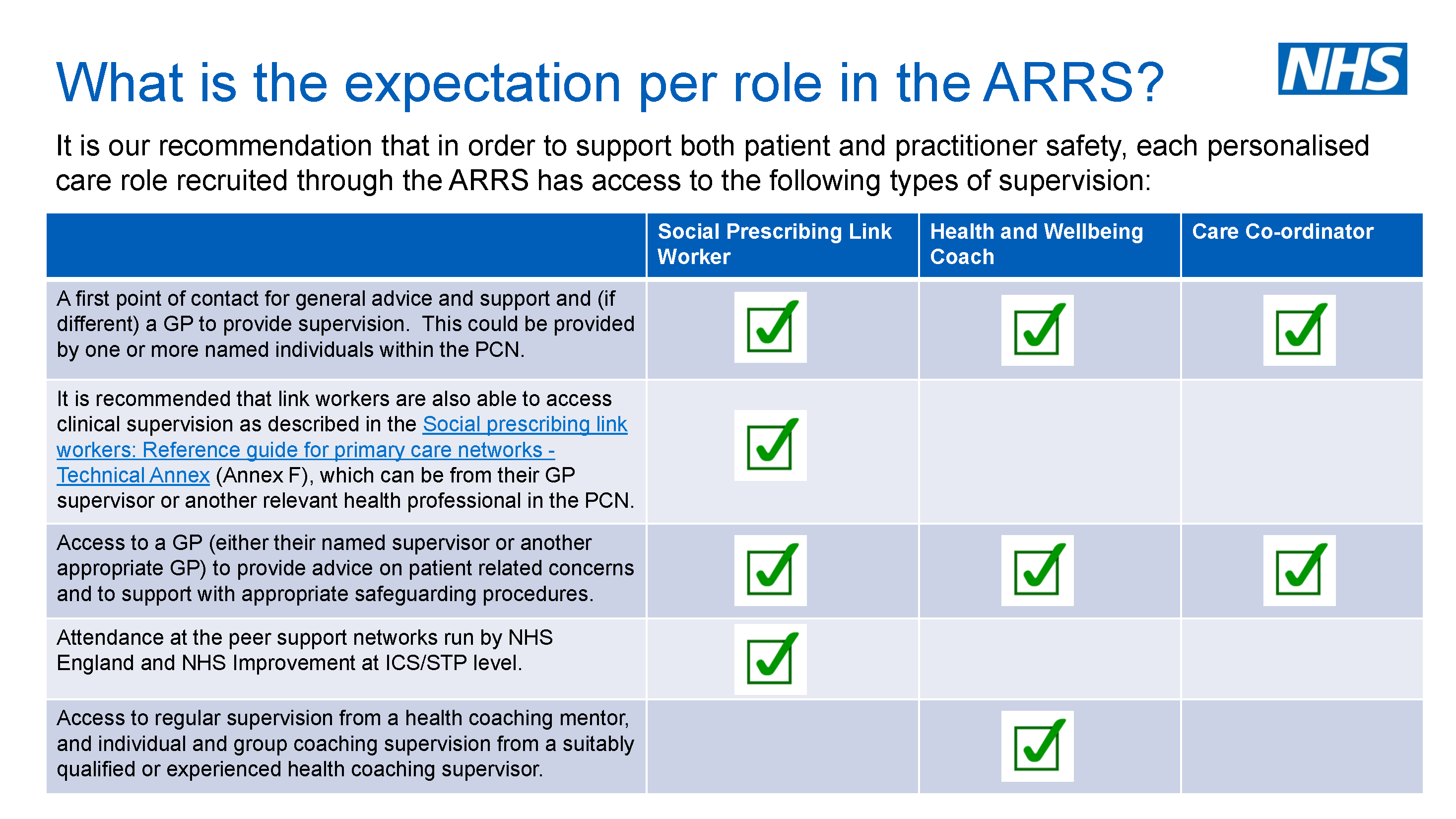
- Page 38 of the Network Contract Direct Enhanced Service (DES) outlines a number of requirements for PCNs that each PCN must comply with in relation to roles recruited through the ARRS scheme, including a specific request for “access to appropriate clinical supervision and administrative support.”
- Supervision can take a variety of forms to be effective. The right level of supervision is vital for both staff and patient safety, and has additional benefits including staff retention as staff who feel supported in their role are also more likely to stay in post
- There are different types of supervision including managerial and clinical supervision:
– Clinical supervision is provided primarily by a GP or qualified advanced practitioner to discuss complex cases, for reflection and restorative support
– Managerial supervision may be provided by a PCN manager of HR professional for HR issues
– Community Services supervision operates in some areas in addition to other forms of supervision to support ARRS professionals to build links with and access community support for complex patients
– For HWBCs line management and clinical supervision can be provided by any (and the same) HCP but coaching supervision must be provided by an accredited professional - Regularly schedule supervision and ensure there is a named clinical supervisor
- Ensure there is a named GP or other HCP on the day in the practice to provide support on urgent/emergency cases and/or debrief
- Ensure supervision time is protected for both the personalised care role and supervisor- it is essential that this is ringfenced
- Consider joint clinics with a GP/ HCP to support identification of learning needs and building skills and confidence
- Hosting MDTs with an educational component can be useful for multi-professional learning and reflection
- Encourage attendance at peer support networks run by NHSE/I and regionally
- Creating a local support peer support across neighboring PCNs can encourage personalised care roles to come together, reflect and learn from each other, as well as increase a sense of belonging and build professional solidarity
- E- learning for Health module on supervision for SPLWs may be of interest to GPs and other HCPs providing supervision to personalised care roles, covering areas such as:
- How to provide a safe and protected time for support and learning through in-depth reflection.
- The purpose and various functions of supervision: formative, normative, restorative.
- How to structure a clinical supervision session and what preparation may be helpful.
NHSE has created a resource jointly with HEE to support PCNs to provide supervision to ARRS roles including case studies of PCNs who have developed innovative supervision practices.
Wellbeing support for the workforce, the offers from Healthy London Partnership can be found on our website here.
Social prescribing link workers
SPLWs deal with the social determinants of health, by working with people to understand what changes they want to make and supporting them to link into community assets and services to do this. By addressing the social determinants of health, SPLWs are critical to eliminating health inequalities.
There are currently over 70 Social Prescribing Programmes and more than 450 SPLWS in London. The London Social Prescribing Map is a useful resource to support the visibility of service models with key contacts for networking and good practice sharing across London.
To read more about how social prescribing link workers are being used to address health inequalities in London, you can read this blog.
Care coordinators
Care coordinators can be used for proactive case finding, working with complex patients and supporting healthcare access, navigation and continuity. They support engagement and utilisation of health care services by vulnerable and underserved patient cohorts who experience barriers to accessing healthcare.
To hear about care coordinators in more depth and how they can be used to address health inequalities, watch back the London spotlight on Care Coordinators event here. Slides here. FAQ about employing Care Coordinators can be found here.
Health and wellbeing coaches
HWBCs work with individuals to motivate them to reach specific health and wellbeing goals through structured behaviour change and coaching techniques. They facilitate early intervention, create agency and ownership and provide resources to encourage self-supported management for patients at risk of or experiencing health inequalities through 1:1 or group support with greatest benefits seen for those most in need.
To hear about health and wellbeing coaches in more depth and how they can be used to address health inequalities, watch back the London spotlight on health and wellbeing coaches event here. Slides here.
- Give these roles TIME.
- To spend with patients – e.g. caseloads of 200 – 250 per year depending on complexity for SPLWs. Enforce the message that these roles are patient facing and should have a caseload.
- To attend MDT meetings with multi-agency representation which will enable them to proactively case find patients and support holistic care. An educational component can support learning and development.
- To build a meaningful bridge between primary care and the community, scope appropriate activities, influencing development etc. Ringfence time for engaging with services and communities they serve. Some PCNs allocate a weekly community development day for the personalised care roles to build relationships.
- To proactively reach out to cohorts of patients experiencing health inequalities and most in need of this support. Take a population health approach to tailor caseloads. Know about your local population needs.
- To connect with each other, access peer support and ongoing training and development. Empower them to become leaders in personalised care and reducing health inequalities. Some PCNs have weekly community outreach (see Reducing Health Inequalities case study: Health Inclusion and Homelessness in Lewisham).
- Support these roles e.g. supervision, mentoring and training
- Identify clinical leads, GPs and health inequalities leads who can offer supervision and support
- Ensure the three roles are working effectively together so they are being used to their greatest value and can support each other
- Ensure there is a robust plan in place, with induction, clear job roles, ways of working and a plan for development to lead on inequalities
- Communicate to the wider referring workforce, the purpose of the roles, what patients they work with, their value at a practice and PCN level. A clinical advocate for these roles such as GP or PCN health inequalities lead is key
- Identify funding and resources to support health inequalities work – HI DES specification, QOF, IIF, ARRS underspend, community grants, co-commissioning models
- Support them with clinical and personal supervision and a opportunities for learning and development so they are equipped to support complex patients and empowered to develop projects that support the wider practice and PCN. See resource box below for training and learning opportunities.
Read our case study on developing a health inequalities strategy in Sutton.
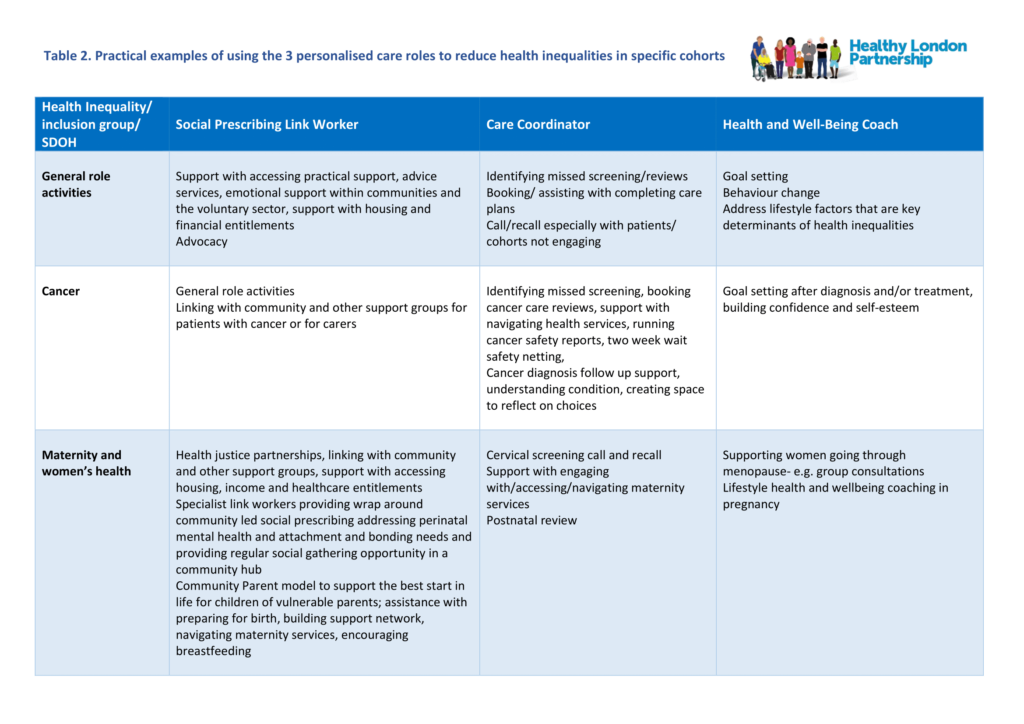
Table 2 shows practical and specific ways the three personalised care roles can be used to reduce health inequalities by using a CORE20PLUS framework and combining a population health, proactive outreach and one team approach.
Click the table below to open in a larger readable format – Practical examples of using the 3 personalised care roles to reduce health inequalities in specific cohorts table
Read more in our case studies series:
- All the roles are focused on supporting patients to address what matters to them in a holistic way.
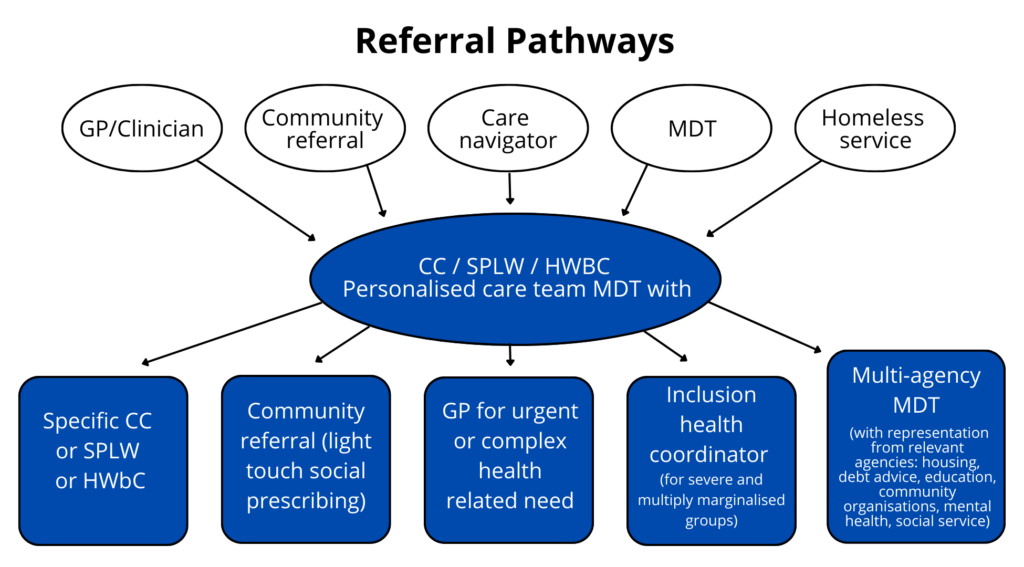
- One of the challenges that PCNs have reported is how to best use the roles in a way that ensures clear referral processes and draws on the unique skills and strengths of each role individually but also recognises the complementarity and fluidity between them.
- A “one team personalised care approach” is being adopted in some PCNs. The diagram below shows what a referral process can look like, with SPLWs being the main port of entry.
- In practice, however, PCNs are using the one team approach in a much more versatile way, adapting to local needs and resources to enable greater reach and impact. Examples are given below.
- To hear examples of how the roles are tackling health inequalities individually and together across London, see the slides and recording from this webinar.
Examples of PCNs adopting a “one team approach” for personalised care
Providing personalised care
- Light touch social prescribing by CCs and onward referral to HWBC
- In some PCNs referrals to HWBC also go to SPLWs as usually there is something around social determinants that link workers can help with
- In some PCNs CCs screen initial referrals and then forward them on to HWBC/SPLW.
Referral systems
- Use of system templates for referrals from GPs, nurses and some LWs.
PCN leaflets to communicate information about roles and referral process - Self-initiated meetings by three roles has increased referrals in some PCNs
- SPLW and HWBC work through referrals and refer between each other if initial referral is not appropriate
- Some PCNs have tried to build in a referral system but in others, emails or tasks are main ways of referring as this builds on pre-existing processes.
Learning and supervision
- Two weekly meetings between service lead and all personalised care roles to address any non-clinical issues e.g. workload, supervision set up, day to day duties, opportunities for training and development.
Mixed clinical supervision for LWs and HWBCs once a month - Educational component in MDTs.
MDTs and referral pathways
- Clear referral pathways and criteria are important to ensure appropriate referrals and support referrers. These need to be co-designed with all stakeholders and partners involved
- Monthly ARRS meetings led by PCN managers – project manager, service lead, case manager or personalised care leads may also be present depending on structure of the personalised care team
- Weekly meeting with community services and personalised care roles and report to a community-based health inequalities team
- Weekly MDT for CCs and SPLW to collaborate on caseloads, working on a system/ tool to facilitate this
- Involve personalised care roles in multi-agency specialist MDTs such as frailty and paediatrics
Ways of working- quotes
- “Our workloads are quite separate but as we are in the same office once a week we can discuss patients.”
- “We have had a helpful meeting on ways of working, including the in-house pharmacist (as we both get referrals from here too).”
- “All roles month share case studies once a month with the practice team on what they are doing that might be new.”
- “Our SPLWs found out they had CC, so they took initiative to meet regularly with CC which has helped us work better.”
Good referral practices
- Co-design referral pathways with all stakeholders involved and communicate criteria and process to all referrer groups- keep this simple and accessible
- Reach out to/collaborate with neighbouring PCNs for ideas/examples of good practice.
Ensure there is clear consent from the patient being referred and that they understand who the referral is to, the purpose of the referral, time frame for contact and method of contact - Take the patient’s views and preferences into consideration around what they need and want.
Follow local referral processes- templates/emails/tasks documenting the reason for referral, what input is required and timeframe for review - Any communication, physical, disability or cultural requirements of the patient
- Communicate any risk issues which are especially important when working with complex needs patients.
Employing SPLWs
Social Prescribing Technical Annex for PCNs: A guide for PCNs with a framework for link workers and information on recruitment, induction, supervision and learning, care planning, quality assurance, referral systems and measuring impact.
Supporting link workers in primary care: https://www.england.nhs.uk/personalisedcare/social-prescribing/ – full list of resources including
- Summary Guide – gives a clear picture of what a good social prescribing scheme looks like. It also includes a Common Outcomes Framework to help measure the impact of social prescribing on people, the local system, and the voluntary and community sector.
- Reference Guide for PCNs – provides information on setting up social prescribing services including support for recruitment, induction and supervision. It also outlines what quality assurance measures are necessary, and how information can be gathered to help develop a consistent evidence base for social prescribing.
- PCN toolkit (technical annex) provides templates and guides to support PCNs in implementing social prescribing.
- Welcome and induction pack for link workers in primary care networks.
- Handout for practice staff to give to people who are referred to a social prescribing link worker.
- Accredited online training: a list of training through e-learning for social prescribing link workers.
- Social prescribing FutureNHS collaboration platform– online network for sharing resources and for discussion. To join, you can complete a form available here.
Employing HWBCs
- Health Education England guidance – at a glance information about role, funding, training/development and link to case studies.
- Welcome pack for newly appointed health and wellbeing coaches in PCNs: NHSE welcome pack for HWBCs starting in PCNs including training and supervision requirements, support and list of useful resources and training.
- Health coaching guide and technical annexes: implementation and quality guide to support the commissioning and delivery of health coaching aimed at commissioners and system leaders including implementation checklists, practice examples and minimum standards.
- Health & Wellbeing Coaching- What it is (and what it isn’t)– a useful table of what HWBCs can do and what is not suitable.
- Patient referral suitability– examples of patients suitable for HWBCs.
- Self-supported management guide– overview of self-supported management principles, components, good practice and resources to support local implementation.
Employing CCs
- Welcome pack for newly appointed CCs in PCNs: NHSE welcome pack for CCs starting in PCNs including information on care coordination and self-supported management, role, ways of working, care planning, support and training.
- Health Education England guidance – at a glance information about role, funding training/development, skills and competencies and link to case studies.
See the Healthy London Partnership for more details.